Macrocephaly (Large Head size)
A Structured Approach to Investigating a Child with a Large Head
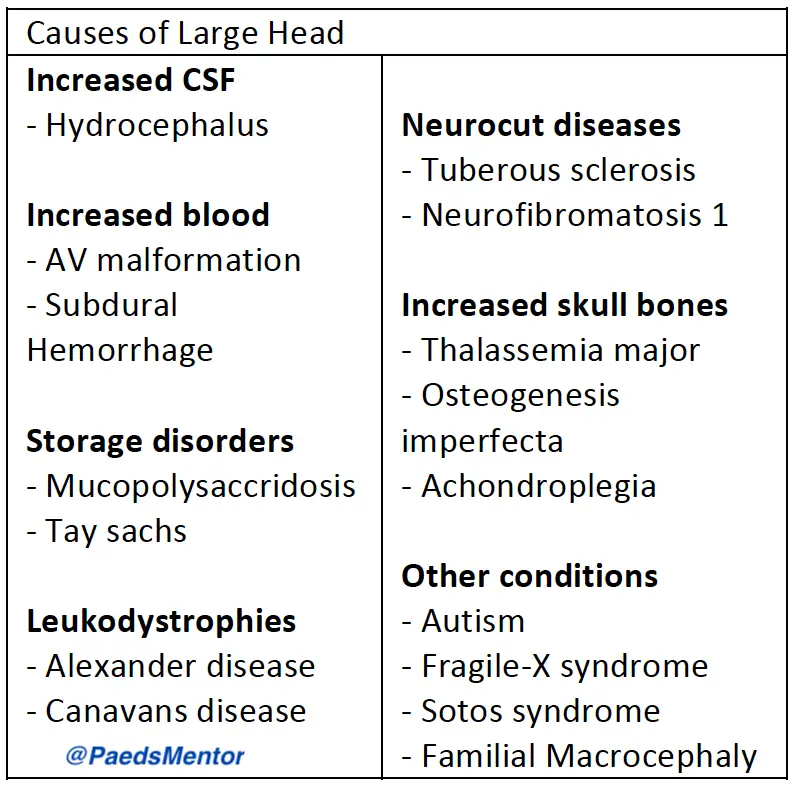
A child presenting with a head circumference that is larger than normal, a condition known as macrocephaly, requires a careful and systematic evaluation. The goal is to determine if the large head size is benign (such as a familial trait) or if it’s due to an underlying pathological condition.
Clinical History: Uncovering the Story
A detailed history helps differentiate between causes of macrocephaly.
Symptom Onset: Was the child acutely unwell? Are there any signs of raised intracranial pressure (ICP), such as headaches, vomiting, or lethargy?
Seizures & Consciousness: Has the child had any seizures or episodes of altered consciousness?
Development: Is there any developmental delay or regression of skills?
Birth History: Inquire about prematurity or any complications in the neonatal period, which could have led to conditions like intraventricular hemorrhage.
Family History: Ask about head sizes in the parents and other family members, as benign familial macrocephaly is the most common cause. Also, ask about a family history of neurometabolic diseases.
Physical Examination: Looking for Clues
The physical examination is crucial for finding the cause.
Head Circumference: Plot the child’s occipitofrontal circumference (OFC) on a growth chart and compare it to their parents’ head size.
Signs of Raised ICP: Look for a bulging fontanelle, separated sutures, or other signs of hydrocephalus, such as ‘sunset eyes’ or dilated scalp veins.
Physical Features: Examine the head shape for symmetry and look for any dysmorphic features or midline deformities that may suggest a genetic syndrome.
Neurocutaneous Signs: Carefully check the skin for any neurocutaneous signs (e.g., café-au-lait spots) using a Woods lamp.
Neurological Assessment: Perform a full neurological exam, assessing for spasticity, abnormal tone, or reflexes. A formal developmental assessment is also essential.
Other Systems: Check for hepatosplenomegaly or other systemic signs that may point to a metabolic disorder.
Investigations: Confirming the Cause
Investigations are guided by the clinical findings.
Neuroimaging:
Cranial Ultrasound (CrUSS): This is the first-line imaging for infants with an open fontanelle.
MRI Brain: An MRI provides detailed structural information and is the gold standard for investigating the cause of macrocephaly. It helps differentiate between hydrocephalus, megaencephaly (an enlarged brain), and other pathologies.
CT Head/Skull X-ray: These are considered if you suspect conditions like craniosynostosis (premature closure of the skull sutures).
Selective Testing:
Genetic Screens: A microarray may be considered if there are dysmorphic features, developmental delay, or other congenital malformations.
Neuro-metabolic Tests: These are performed selectively to rule out metabolic disorders.
Other Imaging: An abdominal ultrasound or echocardiogram may be considered if systemic issues are suspected.
Management: Tailored to the Diagnosis
Management is tailored to the specific diagnosis.
Benign Familial Macrocephaly: No intervention is needed beyond reassurance and routine monitoring.
Hydrocephalus: Manage raised ICP medically (e.g., Mannitol) or surgically with a ventriculoperitoneal (VP) shunt or other procedures.
Symptom Management: Treat any associated symptoms like seizures or spasticity.
Developmental Support: Ensure the child receives appropriate developmental support, including therapy services.
Referrals: Refer to specialists like genetics, neurosurgery, or ophthalmology as needed.
