Lymphadenopathy in Children
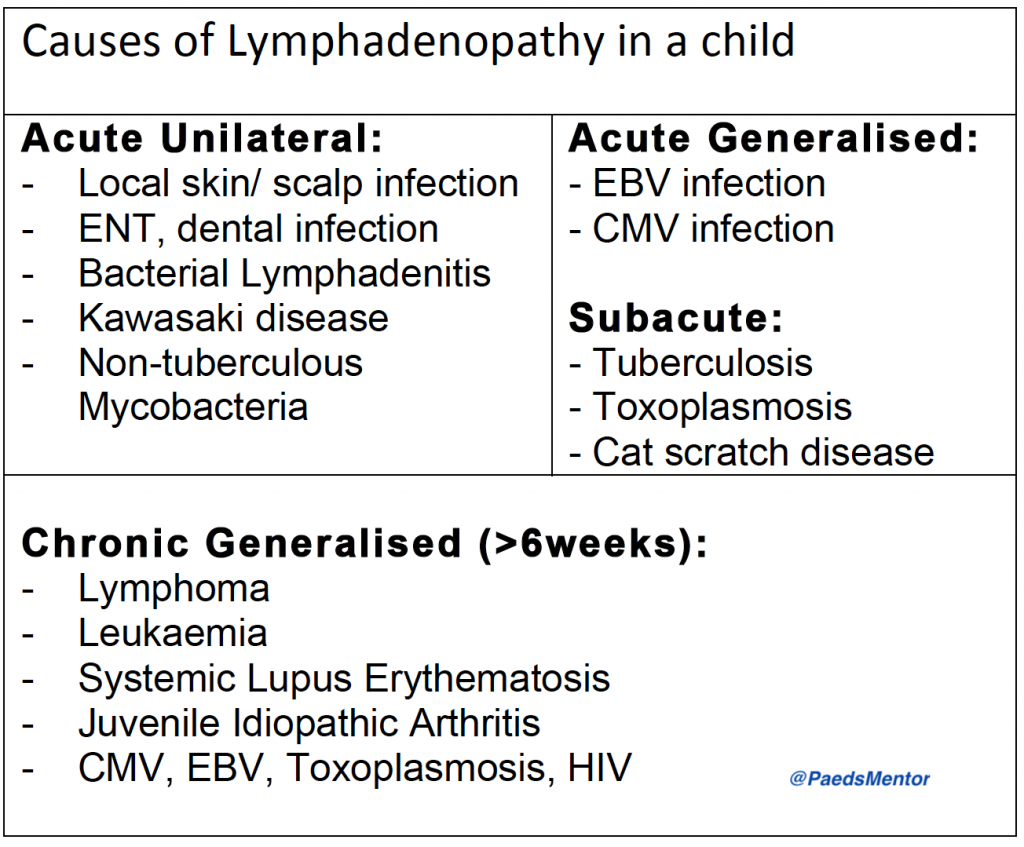
Lymphadenopathy, or enlarged lymph nodes, is a frequent reason for paediatric referrals. While most cases are a benign, self-limiting response to a localised infection, a careful and systematic assessment is crucial to rule out more serious underlying conditions, such as malignancy or systemic disease.
Clinical Assessment
History
A detailed history is the cornerstone of the assessment. Key questions include:
Characteristics of the lymph node: How many are enlarged? Are they tender or painful? Is there any associated redness?
Systemic symptoms: Ask about fever, night sweats, weight loss, or fatigue.
Source of infection: Inquire about a sore throat, dental pain, cough, or a skin infection.
Specific exposures: Ask about recent travel, exposure to animals (e.g., cats for cat scratch disease), or a family history of tuberculosis.
Red flag symptoms: Screen for signs of a serious illness, such as pallor, bruising, bone pain, or a limp.
Examination
A full physical examination is essential.
General appearance: Is the child well, or do they look unwell or pale?
Lymph node description: Note the size, location, and whether the nodes are unilateral, bilateral, or generalised. Palpate the nodes to determine if they’re tender, fluctuant (suggesting an abscess), firm, rubbery, or matted (stuck together). A rubbery, hard, or matted lymph node is a major red flag.
Systemic exam: Perform a thorough ENT examination. Check the skin for rashes or eczema. Assess for hepatosplenomegaly, which suggests a systemic process.
Red Flags
Certain features should raise concern and prompt urgent investigation and referral:
Persistent growth: A lymph node that continues to grow for more than two weeks.
Size: A node that remains >2 cm after 4-6 weeks or fails to reduce to <1 cm after 8-12 weeks.
Location: A supraclavicular lymph node is a major red flag for malignancy.
Associated symptoms: Persistent fever for more than two weeks, night sweats, unexplained weight loss, or signs of bone marrow suppression (e.g., bruising, pallor).
Systemic signs: The presence of hepatosplenomegaly.
Management
Management depends on the clinical picture and the presence of red flags.
Acute, Localised Lymphadenopathy
If a local source of infection is suspected, such as bacterial tonsillitis or a skin infection, a course of empirical antibiotics is appropriate. The child should be reviewed in 48 hours.
If a child presents with fever and has a clear focus of infection, but appears well, they can be managed with close monitoring.
Chronic Lymphadenopathy (after 6 weeks)
Well child with no red flags: If the child is well and the lymph nodes are mobile and non-concerning, they can be safely discharged with clear advice to return if any red flags develop.
Child with red flags: A full work-up is required. This should include:
Bloods: A full blood count with film, U&E, LFT, uric acid, and LDH.
Serology: Testing for viral causes such as EBV, CMV, and Toxoplasmosis.
Imaging: A chest X-ray and an ultrasound of the affected nodes and abdomen/pelvis.
A lymph node biopsy is the definitive diagnostic tool and should be considered if the node is >2 cm, firm or matted, or if there is a strong suspicion of malignancy or a systemic cause. Referral to a paediatric oncologist or ENT surgeon is crucial in these cases.
