Hypocalcaemia in Children
Hypocalcaemia, a total serum calcium level below 2.2 mmol/L (or ionised calcium <1.1 mmol/L), is a significant electrolyte imbalance in children. Ionised calcium is the physiologically active form, and its measurement, along with albumin, is crucial for an accurate diagnosis. The clinical presentation and management depend on the underlying cause, which is often related to a deficiency in vitamin D, parathyroid hormone (PTH), or magnesium.
Causes
Hypocalcaemia in children can be caused by a variety of factors:
Prematurity: Preterm infants have limited calcium and vitamin D stores.
Nutritional:
Vitamin D Deficiency: The most common cause of hypocalcaemia in children. This can lead to nutritional rickets, where bones become soft and weak.
High Phosphate Intake: Feeding infants with high-phosphate-containing milk formulas can cause calcium to bind with phosphate, leading to low serum calcium.
Endocrine:
Hypoparathyroidism: Inadequate PTH production, which can be seen in genetic conditions like DiGeorge syndrome.
Pseudohypoparathyroidism: The body’s tissues are resistant to PTH, even though levels are normal or high.
Drugs: Certain medications, such as phenytoin and cisplatin, can interfere with calcium metabolism.
Other Causes: Hypomagnesaemia is a common cause of hypocalcaemia because magnesium is required for the action of PTH.
Clinical Presentation
Symptoms of hypocalcaemia vary and are often more pronounced with a rapid fall in calcium levels.
Neonates: May present with non-specific signs like poor feeding, vomiting, irritability, or jitteriness. Seizures are a serious and common presentation in this age group.
Older Children: Classic signs of neuromuscular irritability include:
Carpopedal spasms: Involuntary contractions of the hands and feet.
Tetany: Muscle spasms and cramps.
Paraesthesia: A tingling or “pins and needles” sensation.
Positive Chvostek’s sign: Tapping on the facial nerve just in front of the earlobe causes twitching of the facial muscles on that side.
Positive Trousseau’s sign: Inflating a blood pressure cuff above systolic pressure for three minutes induces carpal spasms.
Cardiovascular: Severe hypocalcaemia can lead to a prolonged QTc interval on an ECG, increasing the risk of cardiac arrhythmias.
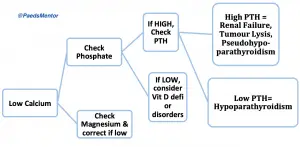
Investigations and Management
Diagnosis:
Initial blood tests should include total calcium, albumin, phosphate, magnesium, alkaline phosphatase, PTH, and 25-hydroxyvitamin D levels.
An ECG is essential to check for a prolonged QTc interval and other arrhythmias.
Acute Management:
Symptomatic hypocalcaemia (e.g., with seizures or tetany) is a medical emergency. The treatment is an intravenous infusion of calcium gluconate given slowly under continuous cardiac monitoring. Extravasation of calcium gluconate can cause tissue necrosis, so a good-quality IV line is crucial.
If hypomagnesaemia is also present, it must be corrected as hypocalcaemia will be refractory to treatment without adequate magnesium levels.
Long-term Management:
For asymptomatic hypocalcaemia, oral calcium and vitamin D supplementation are typically sufficient.
The underlying cause must be addressed, such as treating rickets with oral Cholecalciferol (vitamin D3) or managing hypoparathyroidism with vitamin D analogues like Calcitriol.
