Paediatric Hypertension
Hypertension in children is a sustained elevation of blood pressure (BP) that is above the 95th percentile for their age, sex, and height. It’s an important finding as it can be a sign of a serious underlying condition. The UK approach emphasizes accurate measurement, a thorough search for secondary causes, and early intervention to prevent long-term cardiovascular damage.
Measurement and Definitions
Accurate Measurement: Proper technique is crucial. Ensure the child is calm, sitting comfortably, and the correct cuff size is used. A cuff that is too small will give a falsely high reading.
Classification:
Elevated BP: Systolic and/or diastolic BP between the 90th and 95th percentiles.
Hypertension: BP consistently at or above the 95th percentile.
Hypertensive Emergency: Severely elevated BP with end-organ damage (e.g., encephalopathy, seizures, heart failure).
Causes and Assessment
Unlike adults, hypertension in children is rarely “primary” (essential hypertension), especially in younger age groups. It is most often secondary to an underlying condition.
History
Presenting Symptoms: Ask about headaches, dizziness, nosebleeds, and visual disturbances, which can be signs of a hypertensive crisis.
Medical History: Enquire about a history of urinary tract infections (UTIs) or known renal and cardiac conditions, as renal disease is the most common cause of secondary hypertension.
Medications: Ask about medications like corticosteroids or substance abuse, which can cause elevated BP.
Family History: A family history of hypertension, cardiovascular disease, or kidney disease is a key risk factor for primary hypertension.
Examination
General: Assess for signs of an underlying condition. Look for dysmorphic features (e.g., in Williams syndrome), short stature (suggesting chronic renal disease), and signs of endocrine disorders like Cushing’s syndrome (truncal obesity, “buffalo hump”).
Cardiovascular:
Four-Limb BP: Measure BP in all four limbs. A BP that is significantly lower in the legs than the arms is a classic sign of coarctation of the aorta.
Pulses: Check for a radial-femoral pulse delay.
Abdomen: Palpate for an abdominal mass, which could indicate a kidney tumour (e.g., Wilms’ tumour) or hydronephrosis.
Fundoscopy: Check for signs of chronic hypertension, such as haemorrhages or papilloedema, which indicates raised intracranial pressure.
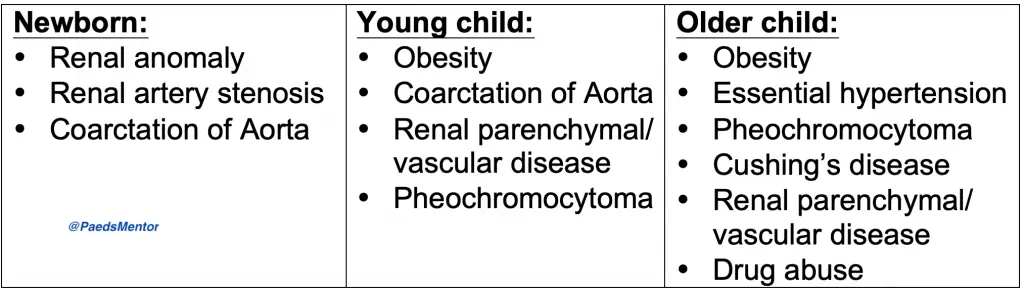
Common Causes
Renal Disease: This is the most common cause. Examples include chronic kidney disease, glomerulonephritis, or renal artery stenosis.
Endocrine: Cushing’s syndrome, phaeochromocytoma, or hyperthyroidism.
Cardiac: Coarctation of the aorta.
Obesity: A major cause of primary hypertension in older children and adolescents.
Neurological: Raised intracranial pressure due to a tumour or infection.
Investigations
Initial Screen:
Blood Tests: Full blood count, electrolytes, urea, creatinine, and thyroid function tests (TSH).
Urine Analysis: Urinalysis (for protein, blood) and urine culture.
Imaging: A renal and bladder ultrasound is a crucial first-line investigation to assess for renal disease.
Targeted Investigations: These are performed based on the initial screen and clinical suspicion.
Renal Function: A DMSA scan to check for scarring or a renal Doppler ultrasound for renal artery stenosis.
Endocrine: Plasma renin, aldosterone, or urinary catecholamines.
Cardiac: An echocardiogram (ECHO) to assess for structural heart disease like coarctation of the aorta.
Management
Lifestyle Changes: For elevated BP and primary hypertension, management begins with lifestyle modifications:
Weight Management: Weight loss is a key intervention for obese children.
Diet: Reducing dietary salt intake.
Exercise: Regular physical activity.
Medications: Antihypertensive medications are required for:
Symptomatic hypertension.
Hypertensive emergencies.
Secondary hypertension with end-organ damage.
Hypertension that is unresponsive to lifestyle changes.
Common Drugs: The choice of medication is dependent on the cause.
ACE inhibitors (e.g., captopril) and angiotensin receptor blockers (ARBs) are often first-line.
Calcium channel blockers (e.g., amlodipine, nifedipine) and beta-blockers (e.g., atenolol, labetalol) are also commonly used.
In a hypertensive emergency, intravenous medications like labetalol or nitroprusside may be required.
Monitoring: Regular monitoring of BP and end-organ function (e.g., renal function, echocardiogram) is essential.
How to confirmation Hypertension in a child using BP centiles?
Finding BP centiles for children isn’t as straightforward as using a single chart for all ages. It requires using a specific chart based on the child’s age, sex, and height. The easiest and most reliable method is to use a digital calculator or an online tool that incorporates the complex data from the UK’s BP centile charts.
Here’s why you can’t just use a simple chart and why a digital tool is best:
Variables: A child’s blood pressure is measured against a reference that accounts for their age, sex, and height. This means a single BP reading can be normal for a tall 10-year-old but high for a short 10-year-old.
The 95th Percentile: The threshold for hypertension in children is a BP that’s consistently at or above the 95th percentile for their age, sex, and height.
UK Guidelines: Medical professionals in the UK use specific reference charts based on international data. These charts are complex to use manually because you have to plot the child’s height against their age to find the correct BP centile curve.
A practical solution for medical students and trainees is to use a mobile app or a website with a paediatric BP centile calculator. You simply input the child’s age, sex, height, and BP reading, and the tool gives you the exact centile. This eliminates the risk of misreading a complex chart and is the standard of care for accurate assessment.
